Health spending in the Philippines has more than doubled over the past decade, crossing PHP 1 trillion in 2021 and expected to reach PHP 1.4 trillion in 2024—experts warn that a fragmented, unevenly run health system is holding back Universal Health Care (UHC).
During the second session of the “UHC in Numbers: A Forum on the Philippines’ Progress in Universal Health Care” forum on November 20, 2025, organized by the ��ý (��ý) through its Health Economics and Finance Program (HEFP), it was revealed that the LGUs’ varying priorities and capacities produce inequities in access and inefficiencies in service delivery.
Spending is Rising but health outcomes remain uneven
��ý Senior Research Fellow and HEFP Program Director Dr. Valerie Gilbert Ulep emphasized that the scale of health spending has fundamentally shifted.
“Health spending has more than doubled over the past decade, even after adjusting for inflation and population growth,” he said, noting that per-capita spending has risen from around PHP 3,000 in 2000 to nearly PHP 12,000 today—“a four-fold increase in real terms.”
However, Ulep cautioned that this growth has not guaranteed equitable or efficient access to healthcare.
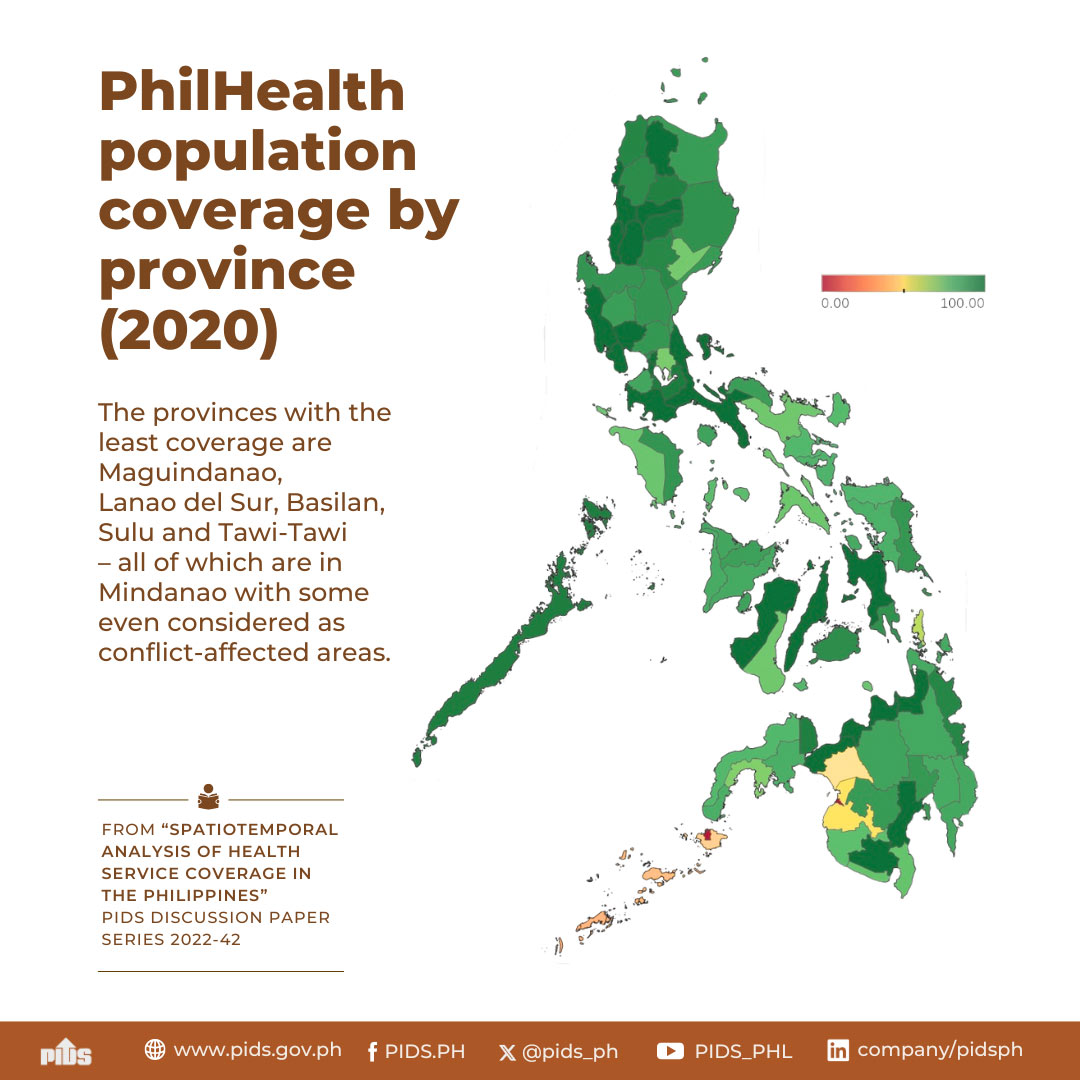
Government spending remains the primary driver of the increase, but local health outcomes continue to diverge sharply because of structural weaknesses at the local level. This fragmentation, combined with inconsistent pricing and varying service availability across LGUs, results in uneven primary care delivery.
The complex mix of financing streams—LGU budgets, PhilHealth reimbursements, national grants, and discretionary funds—further deepens these disparities. Ulep warned that such overlapping sources “exacerbate inequity,” arguing that UHC requires not just larger budgets, but systems designed to ensure coherent, coordinated, and equitable health service provision nationwide.
Infrastructure gaps persist
��ý-HEFP Research Specialist Ms. Therese Jules Tomas emphasized that while overall health spending has increased substantially, investments in infrastructure remain uneven.
“Bed capacity is not keeping up with population growth,” Tomas noted, a gap that reflects the wider challenges of uneven infrastructure development across regions.
Tomas explained that decentralization placed the responsibility for health capital outlay on LGUs, yet actual local spending remains low.
These disparities highlight the limits of relying solely on local resources. Tomas emphasized that variations in LGUs’ financial capacity and technical expertise have led to inequitable access to hospitals, primary facilities, and medical equipment—issues HFEP was designed to address since its launch in 2008.
She stressed the need for stronger monitoring systems, clearer investment criteria, and alignment of HFEP with province-wide health priorities to ensure that capital investments translate into functional and equitable health services.
Human resources remain thin and uneven
��ý-HEFP Technical Specialist Mr. Louie Iyar Dagoy noted that only 3% of the national workforce of health professionals, and more than half of them are in the private sector.
“Areas with higher poverty tend to have fewer health workers per 1,000 population,” Dagoy revealed in their analysis, limiting access to quality healthcare.
Despite higher salaries, public-sector physicians face heavier workloads, reflecting systemic inefficiencies and chronic understaffing.
Dagoy urges the creation of a national HRH support system, along with a well-coasted global budget system approach for public facilities.
“Universal care cannot succeed without a well-compensated, well-supported, and well-motivated HRH workforce,” he stressed.
Weak information systems undermine reforms
Complementing workforce and infrastructure, ��ý-HEFP Technical Specialist Mr. Jomelle Wong emphasized the need to strengthen Health Information Systems (HIS) to improve healthcare delivery across the country.
He mentioned that fragmented systems, ambiguous governance, and insufficient technical support hinder effective HIS implementation.
“The entire health sector is investing in HIS, but the technical unit in DOH for HIS is getting smaller,” Wong noted.
Limited training and reliance on paper-based systems further reduce system utilization, leaving facilities unable to optimize available tools.
Wong’s advocated for clear governance roles, interoperable systems, and comprehensive support for facilities.
“It's not about simply doling out a computer with the software, it's about providing the suite of things that ensure services are delivered end-to-end,” he stressed.
Systemic challenges and reform strategies
The presentations set the stage for a broader discussion in the panel, which examined systemic challenges and reform efforts.
DOH Former OIC Secretary of Health Dr. Maria Rosario Singh-Vergeire highlighted persistent gaps in the Philippines’ health facilities despite 15 years of investments. Many barangay health stations remain non-operational, while smaller hospitals lack adequate funding.
Meanwhile, Zuellig Family Foundation Chairperson Dr. Manuel Dayrit highlighted inefficient spending and fragmented governance. Capital investments often fail to account for staffing or equipment needs, creating underutilized facilities.
WeSolve Foundation President Mr. Kenneth Isaiah Ibasco Abante highlighted the need to address corruption in health spending, describing it as a “cancer” hindering progress. He called for empowering civil society, LGUs, and researchers to track budgets and projects.
World Health Organization-Philippines Health Systems Strengthening Team Coordinator and Team Lead Dr. Yu Lee Park emphasized financing reform as a critical driver of UHC. Drawing from Thailand and Mongolia’s experience, she highlighted how pooled funding and strategic purchasing can strengthen primary care.
Translating Evidence into Actionable UHC Reforms
In closing, DOH Development Bureau Director Johanna Banzon said that the insights shared throughout the session reflected the realities faced by Filipino families and the frontline workers who serve them.
“Behind every data set is a Filipino family making difficult decisions. Behind every indicator is a health worker trying to serve, and behind every statistic is a life we can make better,” she noted, underscoring the human impact behind the numbers.
Banzon stressed that achieving UHC will require stronger collaboration across national agencies, LGUs, civil society, and development partners; more coherent and accountable financing; and a commitment to evidence-informed action.
She urged stakeholders to work collectively toward building a health system that is fair, responsive, and centered on the needs of every Filipino.
To learn more about the studies, visit the ��ý-HEFP website: . Watch the recording of the forum session here: .###—RTG